An interview with prof. dr. Martin Boeree
A considerably higher dose of the anti-tuberculosis drug rifampicin has been found to be safe according to a recent publication by PanACEA. Higher dosing of rifampicin may lead to a shorter / more efficacious treatment for tuberculosis with less resistance development. With this finding PanACEA researchers complete a decade-long search for the right dosing of rifampicin.
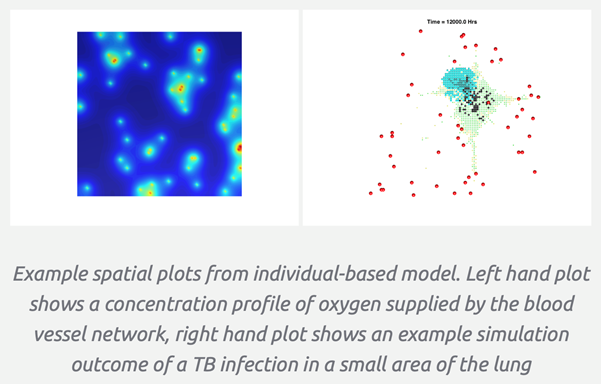
One of the few effective drugs against tuberculosis is rifampicin. Even after fifty years, this remains one of the few anti-tuberculosis drugs that penetrates all parts of the body, including those hard-to-reach areas where the tubercle bacillus resides. Yet all this time, patients have been receiving too low a dosage, of only 10 milligrams per kilogram of body weight.
“A higher dose was too expensive at the time of introduction, people were afraid that the drug would be toxic, and in 95 percent of cases the dose was sufficiently effective,” says Boeree. “That’s why the maximum tolerated dose was never examined. And yet if the dosage is too low, you encourage resistance development in the remaining five percent.”
With this recent PanACEA publication, the search for the maximum dose of rifampicin is now complete. “We now know that at 50 milligrams per kilo, patients suffer from a kind of general malaise. But a dose of 40 milligrams per kilo does not produce severe side effects.” says Boeree.
Whether a higher dose of rifampicin can actually lead to a shorter treatment duration and less resistance is difficult to say on the basis of their research at this point of time. PanACEA will therefore begin follow-up research this summer to determine the actual outcome of their new treatment strategy. “If we know how many patients have recurrent tuberculosis after a year, and we compare this to a control group, we can make a prediction of how well this new regimen may work,” says Boeree.
“We think that a large proportion of patients will not need six months of rifampicin if we give it at a higher dose,” Boeree says. “It’s quite possible that three months is enough.” If that turns out to be the case, he says, it will have a very big impact in the treatment of tuberculosis worldwide. “The shorter the treatment, the higher the adherence and the lower the resistance. With this study, we can increase the effectiveness of this crucial drug.”
This study is part of the EDCTP2 programme supported by the European Union (grant number TRIA2015-1102-PanACEA).